Pressure ulcers often develop slowly but can develop in just a few hours with the right conditions.
Pressure ulcers are likely to develop faster when there is higher pressure on a smaller area, and more slowly when there is lower pressure over a wider area.
What are the Early Signs of Pressure Ulcer Development?
Early signs of pressure ulcer development include:
- A change in the colour of the skin. People with pale skin are more likely to see red patches on the skin, and people with darker skin area more likely to see purple or blue patches.
- Reddening of the skin that does NOT turn white when you press it. This is called a ‘non-blanching erythema’.
- Any unusual changes in skin texture may be related to pressure damage. Common changes include skin feeling spongy or ‘boggy’.
- A patch of skin that feels cooler or warmer to the touch than others.
- A sore or itchy patch of skin.
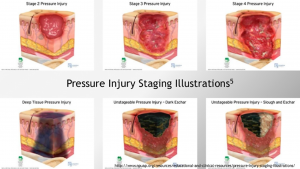
Bedsores fall into one of several stages based on their depth, severity and other characteristics. The degree of skin and tissue damage ranges from red, unbroken skin to a deep injury involving muscle and bone. Skin showing these signs of pressure ulcer development may be referred to as ‘category one’.
See our related article for more information on the staging of pressure ulcers.
What are the Later Signs of Pressure Ulcer Development?
As pressure ulcers worsen, they may break the skin. Signs of worsening pressure ulcers include:
- An open wound or
- A deep wound that reaches the deeper layers of the skin.
- A very deep wound that may reach the muscle and bone.
When should I get help for a Pressure Ulcer?
The NHS website says that if you’re in hospital or a care home, you should tell your healthcare team as soon as possible if you develop symptoms of a pressure ulcer as it will probably continue to get worse if nothing is done about it.
If you’re recovering from illness or surgery at home, or are caring for someone confined to bed or a wheelchair, contact your GP surgery if you think you or the person you’re caring for might have a pressure ulcer.
Get medical advice immediately if there is:
- Red, swollen skin
- Pus coming from the pressure ulcer or wound
- Cold skin and a fast heartbeat
- Severe or worsening pain
- A high temperature (fever) of 38C (100.4F) or above
These symptoms could be a sign of a serious infection that needs to be treated as soon as possible.
For more information about Harvest Healthcare please click here
For more news please visit our Twitter
Or follow us on LinkedIn