While the major factor in the development of pressure injury is pressure itself, shear forces also play a part.
What causes shear and friction?
When you move over a surface and the body remains in contact with it, the skin can be pulled along that surface. You can feel this ‘drag’ effect if you run your hand over something.
This ‘drag’ is caused by friction and leads to a difference in the direction of movement of the skin and the deeper tissues. This difference is called “shear” and is an important factor in pressure ulcer development.
How can shear forces lead to the development of a pressure ulcer?
Shear causes stretching and tearing of blood vessels which reduce blood flow increase blood pooling and can lead to cell damage.
Shearing stops or reduces blood flow more easily than pressure alone (for example, it is easier to cut off flow in a water hose by bending than by pinching it).
Although shear causes tissue damage slightly differently to pressure, the damage produced is the same as with pressure.
Importantly, it is difficult to create pressure without shear, and shear without pressure, so the two usually go hand-in-hand.
For information on how pressure leads to pressure injury, see our article How Pressure Ulcers Develop?
How can repeated friction cause a pressure ulcer?
As well as being a key element of making shear force, friction between the skin and the stationary surfaces such as bedclothes can result in the loss of the top layer of the skin (the stratum corneum).
Think about repeatedly rubbing your skin against a surface – after a time, the skin would start to become red and sore. This is due to friction.
This inflammation can lead to deeper injury or could be the initial damage needed to start pressure ulcer formation.
When there is a loss of the top skin layer, there is also a breach in the barrier against infection.
How can friction and shear be reduced?
There are several strategies to reduce shear and friction forces:
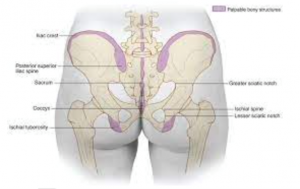
- Use low-friction clothing such as Parafricta undergarments and socks to reduce friction on the vulnerable heel and pelvic areas. These can be especially useful for people who push themselves back up the bed using their heels, or who have involuntary leg movement, for example, those with Parkinson’s.
- Use positioning aids such as slides sheets under the person’s body and feet and heels when repositioning to reduce the risk of friction and shear.
- Use a profiling bed with an in-built knee break. When the person has been repositioned in bed, elevate the knee break first to prevent the person from sliding down the bed.
For more information about Harvest Healthcare please click here
For more news please visit our Twitter
Or follow us on LinkedIn