Pressure ulcers vary in size and severity of the tissue affected, ranging from reddening of the skin to damage to muscle and underlying bone.
How are Pressure Ulcers Staged / Graded / Classified?
According to the international classification system pressure ulcers can be staged as one of six categories.
Superficial
Stage 1: Intact skin with persistent reddening, known as ‘non-blanching erythema’. For more information on non-blanching erythema, click here.
Stage 2: An abrasion or a blister can be seen, without bruising. There is some skin loss or damage affecting the top skin layers.
Superficial ulcers are more difficult to spot than deep ulcers. For information on the warning signs of pressure ulcer development click here.
Deep
Stage 3: Full thickness skin loss which can expose fat in areas where this exists. Damage is limited to the skin and fat layers.
Stage 4: Full thickness skin loss with damage to the underlying structures, such as tendons or bone, which may be exposed.
Other
Deep tissue injury: Tissue injury hidden under intact skin. These appear as deep bruises and can quickly deteriorate into a high-stage pressure ulcer. For more information on why deep tissue injuries occur, click here.
Unstageable Pressure Injury: Pressure ulcer with an undetermined level of tissue injury because the entire base of the wound is covered by slough tissue.
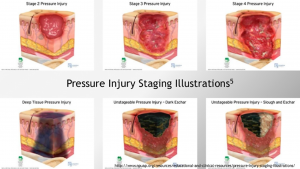
Figure 1 Staging of pressure injury, NPUAP resources
The grading of a pressure ulcer is a critical part of the process of caring for a person with pressure ulcers.
While treatment is tailored to the individual, as may factors can impact the development of a pressure injury, the grade of pressure sore is an important part of creating a treatment/management plan.
For more information on what the risk factors are for developing a pressure injury, click here.
For more information about Harvest Healthcare please click here
For more news please visit our Twitter
Or follow us on LinkedIn